Every year during Suicide Prevention Month, we hear the same messages: check on your friends, reach out if you are struggling, call the suicide prevention number. These messages are certainly important, but at this point, we’ve heard it all so many times that it raises the question if we are really doing enough.
The problem with suicide prevention is that we talk a lot about how to stop people from attempting suicide, but we rarely talk about what happens after an incomplete attempt. While the aftermath of an attempt looks different for everyone, the reality is that it’s often painful, terrifying and even dangerous for some.
As in all 50 states, North Carolina has an involuntary commitment (IVC) law, which makes it possible to legally institutionalize someone who is a danger to themselves or others. For someone to be considered a danger to themselves, they have to be at risk of imminent harm, and that includes intent, a specific plan, access to weapons and a timeframe.
For someone who is truly a danger to themselves, the IVC laws make sense. The problem is that North Carolina has not updated this law in decades, which means that people are involuntarily committed who may or may not be a danger to themselves. Even for those who do need help, most psychiatric hospitals are short-term in nature, and the goal is to stabilize, not to treat. I know because I’ve been there.
In February of my freshman year, I attempted to end my life. I was taken to the emergency room where I was told I would have to be in a hospital for the next 72 hours. I was then taken to a psychiatric hospital where I ended up staying for 14 days.
During this time, I found it incredibly difficult to keep up with my schoolwork; the hospital allowed very limited computer time, and phones were locked up, so I could not use my two-factor authentication and, therefore, could not access Moodle. This, in an addition to the psychological and emotional toll of being hospitalized, resulted in my getting behind on schoolwork, which had detrimental effects on the rest of my semester.
This is important for all students to keep in mind because, if you feel you might need to go to a hospital or are referred to one, it is important to have a plan in place, which may include asking professors for accommodations. Also, the Disability Resource Office can provide accommodations for students with a range of disabilities, including mental illness.
It is also important to mention that I was very lucky. Because I have white privilege, I did not have to worry about getting physically assaulted when I was taken to the hospital. However, for BIPOC, this is not the case. Because of racism and the lack of crisis intervention training among police officers, Black people who encounter the police during a mental health crisis often face tragic results, which can be seen with Elijiah McClain and Damian Daniels.
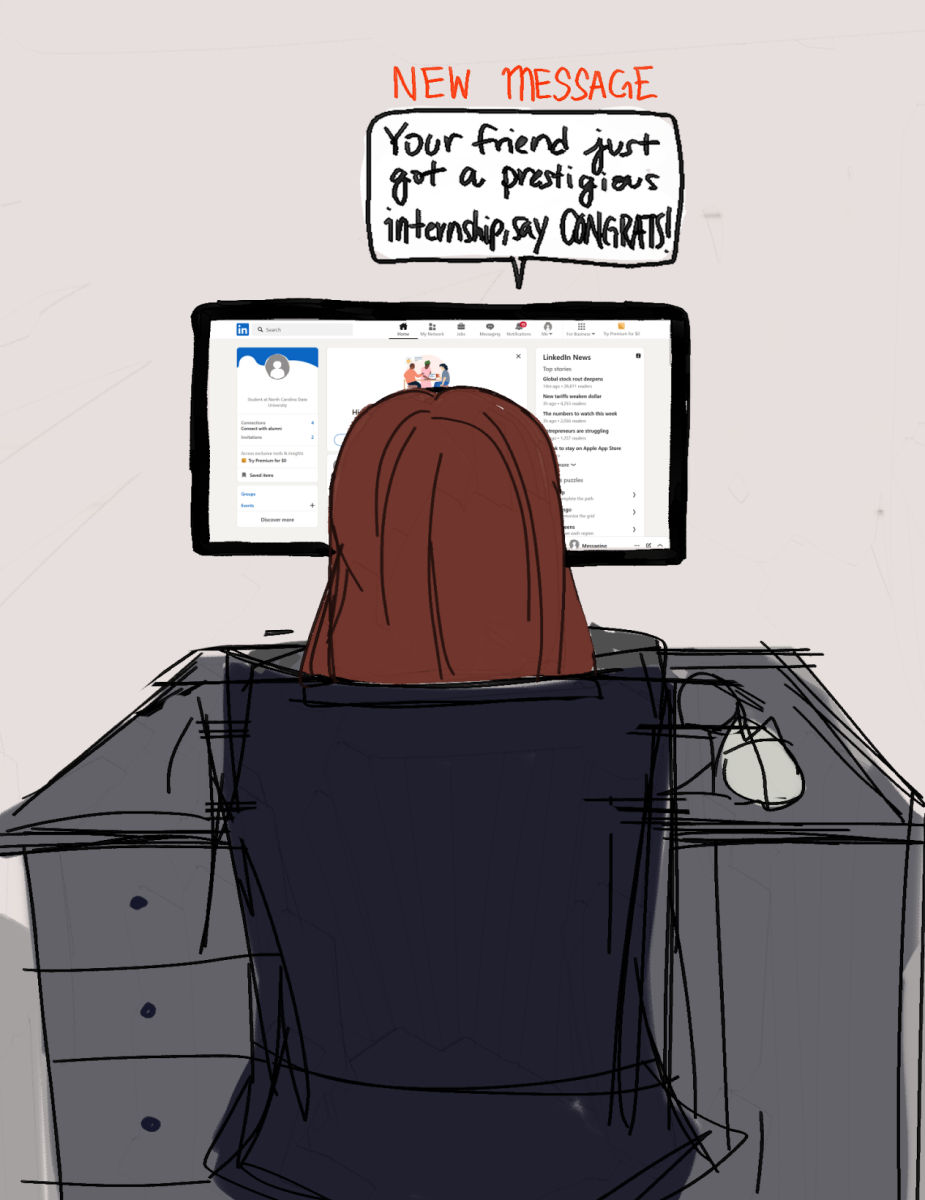
If we are going to end the stigma around suicide, we need to talk about the full story, not just the overused platitudes that (well-intentioned) people post on social media each September. In traditional suicide prevention messages, it seems like the point is to almost make us feel guilty for not checking in on on friends enough, for not being there for people.
But the reality is that, for many people, hospitalization is inevitable, and going to a hospital, whether voluntarily or not, is a scary and even traumatic experience. We need to open the dialogue around hospitalization for mental illness, and, especially for those who struggle with suicidal ideation or have friends who do, it is important to know how the process of involuntary commitment works and have a plan in place in case you or a friend needs to be hospitalized.
It is also important to remember that standard practices like “welfare checks” by police officers can be jarring at best and life threatening at worst for students of color. To prevent suicide, we need to focus on issues like police brutality and health care, which are just as much a part of suicide prevention as any of the messages you read on social media about self-care and checking in with each other.
Without addressing the foundation of the problem, we will not solve it; continuing to focus on surface-level issues while excluding vulnerable populations from the conversation about suicide prevention and ignoring systemic factors that create barriers to getting help for mental illness will only hurt us.