February is National Eating Disorders Awareness Month — four weeks dedicated to raising awareness for a mental health condition that roughly 28.8 million Americans will deal with in their lifetime.
But when people visualize someone with an eating disorder, their mind often paints a picture of an affluent, white cisgender woman with a dangerously low body weight. No one is at fault for having this stereotype; the media is one factor to blame for portraying this character innumerable times in films, books and songs.
Dated research into eating disorders also reinforces this cliche, with many studies concluding that white, young adult women are at greater risk of developing anorexia nervosa or bulimia nervosa. The issue is that these statistics don’t reflect the full picture, and there is a crucial mediating variable at play.
It’s not that upper-middle-class white women are more likely to develop eating disorders — they are just more likely to receive a diagnosis on account of greater access to treatment resources.
When eating disorders are narrowed to a specific population, the doors to proper care are shut to those who don’t fit the mold. Such stigmatizations create barriers to treatment for minority groups — a situation tantamount to a death sentence when dealing with mental illnesses as deadly as eating disorders.
Through increased research on eating disorders over the last decades, studies have found that individuals in the LGBTQ+ community are particularly vulnerable. Renee Avis, a clinician at NC State’s Counseling Center who focuses on eating concerns, said that discrimination, judgment and bullying contribute to this susceptibility.
“It increases isolation, depression, anxiety and they also may not feel like they have a community support that they can reach out to,” Avis said.
Individuals who are transgender deal with body dissatisfaction at an elevated level, putting them at an even greater risk.
“Body image is certainly part of that too, like finding out where and how they feel comfortable in their own bodies,” Avis said.
Men are also typically overlooked as targets of eating disorders under the assumption that harmful beauty standards are exclusive to women. The falsehood of this idea is becoming increasingly apparent, with research showing that an estimated 5-10% of adolescent males and 2% of adult males have an eating disorder.
Bodybuilding and gym culture have fabricated an unrealistic standard for the male physique and are catalysts for what clinicians call muscle dysmorphia, a condition characterized by distress over a perceived lack of muscle mass and tone.
Ariane Machín, the assistant director of Mental Health and Performance Psychology at NC State, said both male and female athletes face a lot of pressure to maintain their physical conditions, presenting a greater risk of developing an eating disorder.
“[Their] bodies are tools in a weird way,” Machín said. “There’s a lot of attention devoted towards [their] bodies and changing their bodies.”
It’s inevitable that many men avoid treatment for eating and body image concerns because of deeply-rooted gender norms. Toxic masculinity discourages men from seeking help and deems mental health struggles as a sign of weakness.
“Sometimes males are less likely to feel as though they’re normal for feeling a certain way or thinking a certain way about their body size and shape,” Machín said.
People of color face considerable underrepresentation in the discussion of eating disorders, yet research has shown that no one ethnic group is more susceptible to eating disorders.
Cultural differences can misconstrue interpretations of eating disorder behaviors, such as East Asian ideals of thinness.
“In some communities, it’s like that’s just kind of the behaviors that happen, and it’s not recognized as being out of the norm or something that needs attention,” Avis said.
In cultures that place more emphasis on physical appearance, the likelihood of individuals receiving treatment for eating disorders is significantly lower, reinforcing the stereotype that only white women develop eating disorders.
To reduce the harmful effects of misrepresentation, Avis said above all, we must normalize the discussion of eating disorders. Through transparency, individuals will feel more comfortable seeking help, even if they don’t fit a stereotype.
“Part of normalizing [eating disorders] is understanding that, for many, it’s a coping strategy that someone has begun using or learned how to use because they’re dealing with other things in their life,” Avis said.
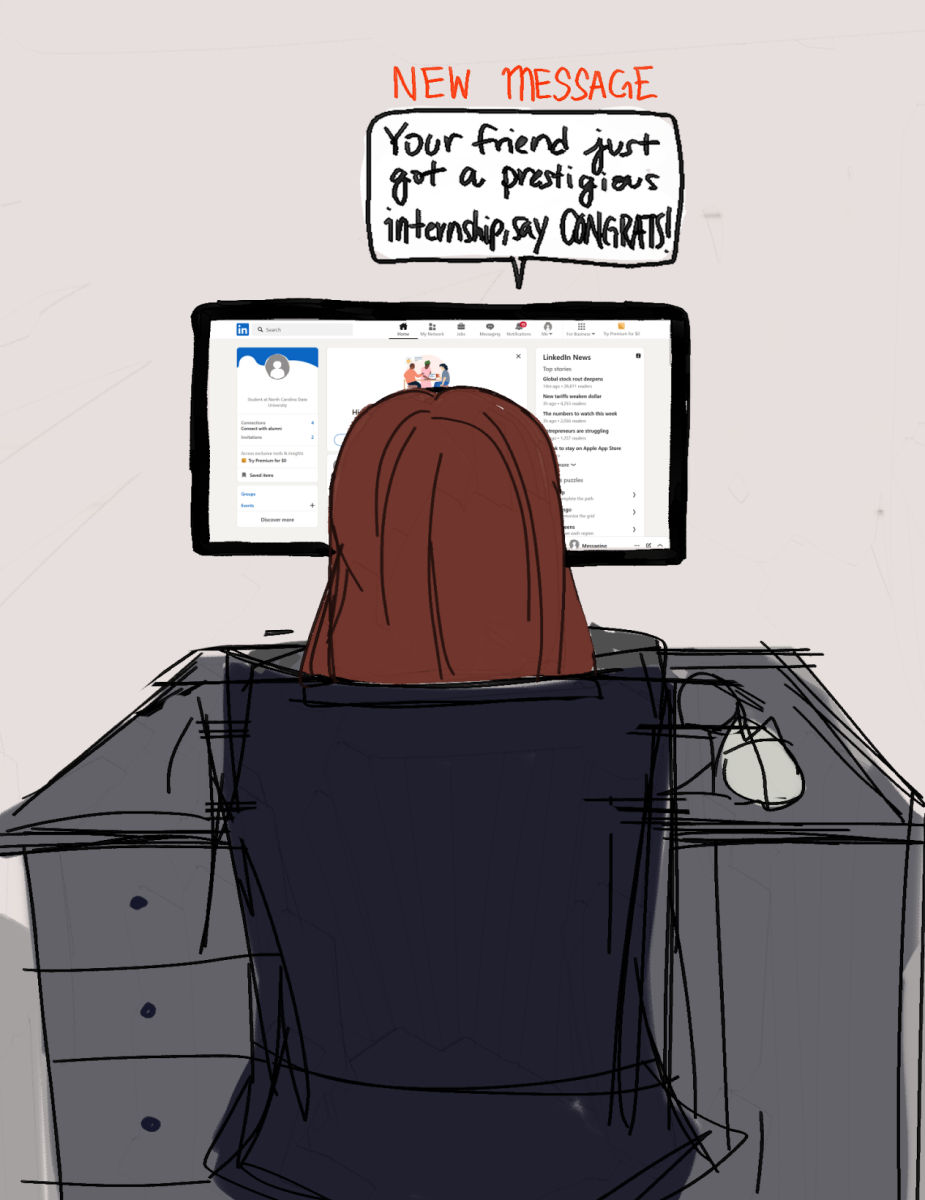
Machín emphasized the importance of vocalizing eating and body-image concerns, even if one does not meet the diagnostic criteria of an eating disorder. Many individuals will struggle with subclinical disordered eating in their lifetime, but addressing those behaviors early on can prevent the development of a clinical eating disorder.
“You don’t have to have an official eating disorder,” Machín said. “Just talk it out a little bit with somebody. It doesn’t have to be a clinician, it’s just to reduce barriers and go from there.”
It’s an unfortunate fact that eating disorders can affect anyone regardless of demographic background, but it’s a fact that requires our attention now more than ever. Eating disorders are non-discriminatory when it comes to who they affect; by recognizing this, we can begin destigmatizing them and improving access to proper care.
If you or someone you know is struggling with an eating disorder, resources can be found through the Counseling Center or NEDA.