Since the late 1970s , when the blood glucose meter was first commercialized, patients with diabetes mellitus have had to prick their skin and test a small drop of blood on a disposable strip to measure their blood sugar level.
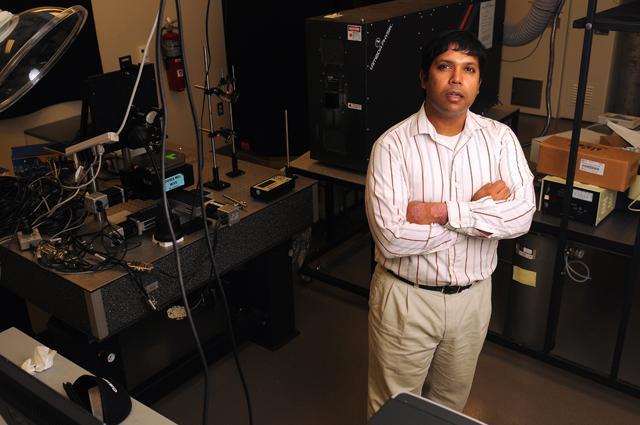
This has been the way of life for well over 30 years but that may all change soon, due to the research being done by our own Dr. Roger Narayan and his team at Sandia National Labs and University of California at San Diego.
Narayan , a professor in the joint biomedical engineering department of N.C . State’s College of Engineering and UNC -Chapel Hill, has integrated microneedles with sensors that can be used for accurate, real-time detection of various chemical levels in the body.
“The end goal is to create a patch device that would simultaneously and selectively detect the physiological chemical changes [in the body] to improve patient care drastically,” Narayan said.
This breakthrough technology would change the way clinicians monitor changes in their patients, and Narayan said it would be extremely easy to use thus making the presence of a health care practitioner would rarely, if ever, be required.
Each unit will only cost five dollars, according to Narayan .
“We want to make this available to everyone, even people in low-income area because the benefit is just too great,” Narayan said.
The method in which Narayan and his team plan to accomplish this is just as advanced.
“We have loaded channels with microneedles and integrated that [ microneedles ] with electrochemical sensors that detect specific levels of pH, glucose, and lactate,” Narayan said. “The long term goal is to use customizable microneedle sensor arrays and incorporate them into wearable devices such as a wristwatch to patients can see their body in a chemical equilibrium at all times.”
Narayan said it’s possible to use smartphone apps as monitors in the future.
Narayan and his team have been working on the biomedical design and prototype for the past 11 months and he said a working prototype will be ready in less than a year.
“My senior design students keep joking with me and ask if the prototype will be ready by April 2012. I always laugh and say there’s no way — although we are working really hard to complete it this year.”
The next step for Narayan’s research is going to be patient application and he hopes that microneedle sensors can be a staple research area for graduate and some undergraduate students.
“The upside is huge, even addition to the numerous clinical applications, this new technology creates various opportunities.”
Narayan referenced an example where the microneedle sensor arrays could be used to track continuous changes in the lactate levels even while people are exercising, compared to measuring the lactate values manually before and after the person exercises.
Narayan said the health risks would be minimal.
“Since the microneedles are invasive, there is a chance of infection because the needles do make pores in the skin,” Narayan said. “We do, however, successfully eliminate the chance for infection by using antimicrobial needle technology which incorporates different metals like silver which protect at the skin-microneedle interface.”
Narayan said he is excited about the scope of the research and expanding the project.
“I think it has the potential to have the same breakthrough effect that the transformation from basic phone to iPhone had on consumers.”